CPR Aid
putting tools in the hands of the people
a collaboration with John Korbin
Page Contents
- Problem Statement
- Goal Outline
- Push Hard
- Push Fast
- Minimize Interruptions
- Costs
- The Device
- References
Problem Statement
According to the American Heart Association, nearly 383,000 out-of-hospital sudden cardiac arrests occur annually, 88% of them in the home, and 70% of Americans may feel helpless to act. That means for a population the size of the UNM student body, more than 35 people will experience cardiac arrest this year and only 10 of them will have a bystander start CPR. Immediate CPR has been proven to be a key factor in post-cardiac arrest recovery, both as an indicator of the likelihood of returning spontaneous circulation and associated with increased neurological function after recovery. Studies have shown that real-time feedback increases rescuer confidence and a confident bystander is more likely to start CPR. The goal of this project is to design a device that will provide real-time feedback for layperson rescuers during non-medical provider cardiopulmonary resuscitation.
Goal Outline
First and foremost, this project aims to meet all the tennants of AHA 2010 layperson CPR, however there are some extra concerns. It is important for this project that the device is easily accesible to people outside of medical careers. As a result, some of the secondary goals of this project include:
- ease of user interface
- low cost
- long shelf-life
- small size
Additionally, as guidelines differ significantly for adult, child, and infant CPR, our first focus will be on a device for adult CPR.
Push Hard
The first of the three main tennants of CPR is to "push hard". This means at least 2" in an adult or 1/3 the depth of the chest in a child or infant. This could be approached from several directions, but it helps to know that the logic behind this is to create a higher intrathoracic pressure in order to "pulse" the vena cava. There are a few ways to measure the adequacy of a compression externally
| benefits | accurate displacement measurement |
small, durable, low power consumption |
easy to manufacture, least tech required |
| costs | bulky, expensive, high power requirement |
backing-material dependent, requires flexible mount |
needs fine calibration, readings may change with heat/use |
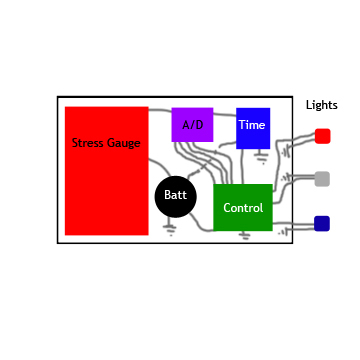
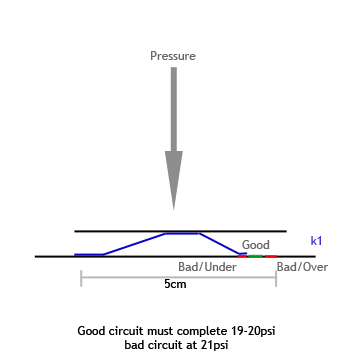
After consideration, the strain gage and spring circuit are those models most likely to fit the needs of the project. Two experimental setups are displayed below.
 |
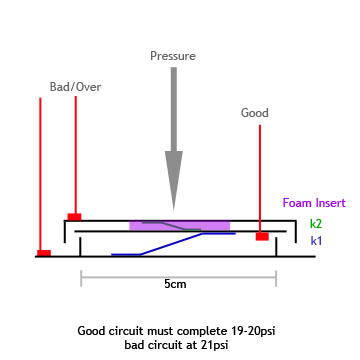 |
| Stress Gage circuit diagram | Spring Circuit side view |
Push Fast
The 2010 AHA CPR guidelines state that a rescuer must compress the chest at least 100 times per minute to be effective at CPR. This generates a rate of 5 compressions every 3 seconds; however it is important to note that no compression will be effective unless the thoracic cavity is given a full chance to recoil before and after. This presents us with two problems to solve:
Compression Rate
We approached the compression rate problem with a simple and elegant solution. A control chip will be required to interpret the data and provide feedback. The timer on the control will be used to count off, like a metronome, and strobe an LED every time a compression is needed.
Chest Recoil
The measure of chest recoil will be based on a reading of zero pressure by the strain gage or spring circuit. The unit will be programmed to read this half-way between the peaks of counted compressions
Minimize Interruptions
The American Heart Association recommends no interruptions. To further this goal, the device will have a feedback light or sound every second compressions are not performed for 10 seconds when it will emit continuous feedback until compressions are resumed.
Costs
Costs for the strain gage design were determined more specifically than the spring circuit design as the spring circuit utilized almost solely salvaged and reclaimed parts, however the strain gage circuit requires purchase of almost entirely novel components. The cost of the casing has not been included as it will vary drastically based on the requirements of each design, but black plastic/vinyl casing from JoAnn's Fabrics could be used enclose each type for roughly $0.10 each.
| Spring Circuit | ||
Spring |
- | donated by Fourslide |
Wiring |
- | Salvaged |
Battery |
$1.07 | Batteries Plus: 3 Volt Lithium Coin Battery - NUCR1632 |
LEDs |
$3.19 | RadioShack: T-1 3/4 5mm Full Color LED Model: 276-028 | Catalog #: 276-028 |
| TOTAL | unknown for prototype | |
| Strain Gage | ||
Controller |
$2.40 | Mouser.com 595-AFE4110B000YS from TI |
Wiring |
- | Unknown, negligible, salvagable |
Strain Gage |
$4.90 | Omega.com case ID 1330240 SGD-1.5/120-LY11 |
Battery |
$1.07 | Batteries Plus: 3 Volt Lithium Coin Battery - NUCR1632 |
LEDs |
$3.19 | RadioShack: T-1 3/4 5mm Full Color LED Model: 276-028 | Catalog #: 276-028 |
| TOTAL | $11.56 | |
The Device
 |
| Modified Spring Circuit |
 |
| Prototype |
| Action Shots (Below) |
| Without Device - unknown quality |
| Insufficient pressure |
| correct pressure |
Through trial and error, the device was created based on a modified spring circuit design. The strain gage version has not yet been fabricated, but will be assembled if this project continues for comparison of reliability and accuracy.
A circuit board was salvaged from outdated hardware and repurposed to form the circuit completions of this design. In fact, for purposes of the prototype, all material used was salvage with exception of the LEDs, battery, and spring (courtesy of Fourslide). Images at the right show the device open and in action.
The prototype itself contains only the spring circuit to provide pressure feedback. An external metronome was used for the purposes of the prototype, however, that will be integrated within the casings in future versions. Three LEDs were used (2 red, 1 green) for pressure indications and a 3v button cell battery powered the entire circuit. No resistors were used in the prototype, but may prolong battery life.
Goal Accomplishment
Not all goals of this project have yet been met. Although the device assists with the "Push Hard, Push Fast" rule of AHA CPR, there is no easy way to help minimize interruptions with this model. That may be easily accomplished with the integrated control chip of the strain gage model. Additionally, the prototype is bulky, but a large part of that is due to the casing which can be easily changed in future versions. Because of the simplicity of this particular design, it was kept at very low cost.
Because the metronome is external and not yet integrated, the ease of use was not very high. Feedback from medical providers trained in CPR indicates that were the metronome integrated, the device would be easy and fairly intuitive to use.
Usage
For providers of CPR, use of the device does not change any of the actions providers take during a rescue attempt. The provider simply slips their hands through the loop on the device before initiating compressions, but otherwise CPR is performed normally as suggested by the AHA.
The beeps of the metronome and its associated light give the timing of compressions at 100 compressions/minute. The triple lights from the pressure sensor light 2 red if pressure is insufficient, 1 green if sufficient, and all three lights if excessive pressure is applied. The rescuer should still perform all other CPR-related activities such as checking for breathing and pulse and especially initiating or instructing another bystander to initiate the emergency response system.
Continued Work
For the future of this device we intend several improvements. As mentioned, we will be integrating the metronome first and foremost. Another priority is to address the "minimize interruptions" portion of the AHA CPR Guidelines. This will likely be accomplished with the use of a capacitor and vibration mechanism on the spring circuit design, but a buzzer or vibration with the strain gage.
A counter/timer will also be added to allow the rescuer to know the number of rounds of CPR performed. Various calibrations may be implemented for use in pediatrics, adults, and geriatrics. In the distant future or with some significant cost increase, a single-use beacon may be added to the device that could notify emergency services that CPR was being performed at the location as triangulated by cell towers.
Ultimately, should this device prove successful, we would like to see it distributed in all CPR classes, used by EMS and other medical personnel and available in every standard first-aid kit.
References
- The American Heart Association
- Sayre, M, Cantrell, S, White, L, Hiestand, B, Keseg, D, Koser, S. Impact of the 2005 American Heart Association Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Guidelines on Out-of-Hospital Cardiac Arrest Survival, Prehospital Emergency Care 2009; 13:469-477. doi: 10.1080/10903120903144965
- Nagele, P. Augmented CPR: rescue after the ResQ trial, Lancet 2011; 311:276-277. DOI:10.1016/S0140-6736(10)62309-4
- Moriwaki, Y, Misugi, S, Tahara, Y, Iwashita, M, Kosuge, T, Harunari, N, Arata, S, Suzuki, N. Complications of bystander cardiopulmonary resuscitation for unconscious patients without cardiopulmonary arrest, Journal of Emergencies, Trauma and Shock I 2012; 5(1):3-6. DOI:10.4103/0974-2700.93094
- Hong, D, Park, S, Lee, K, Baek, K, Shin, D. A different rescuer changing strategy between 30:2 cardiopulmonary resuscitation and hands-only cardiopulmonary resuscitation that considers rescuer factors: A randomised cross-over simulation study with a time-dependent analysis, Resuscitation 2011; 83:353-359. doi:10.1016/j.resuscitation.2011.11.006
- Blinderman, C, Krauker, E, Solomin, M. Time to Revise the Approach to Determining Cardiopulmonary Resuscitation Status, JAMA 2012; 306(9):917-918.
- Yost, D, Phillips, R, Gonzales, L, Lick, C, Saterlee, P, Levy, M, Barger, J, Dodson, P, Poggi, S, Wojcik, K, Niskanen, R, Chapman, F. Assessment of CPR interruptions from transthoracic impedance during use of the LUCASTM mechanical chest compression system, Resuscitation 2012; 30:179-193. doi:10.1016/j.resuscitation.2012.01.019
- Blomberg, H, Gedebor, R, Berglund, L, Karlsten, R, Johansson, J. Poor chest compression quality with mechanical compressions in simulated cardiopulmonary resuscitation: A randomized, cross-over manikin study, Resuscitation 2011; 82:1332-1337. doi:10.1016/j.resuscitation.2011.06.002
- Heidenreich, J, Bonner, A, Sanders, A. Rescuer Fatigue in the Elderly: Standard Vs. Hands-Only CPR, Journal of Emergency Medicine 2012; 42(1):88-92. doi:10.1016/j.jemermed.2010.05.019
- Blewer, A, Leary, M, Esposito, E, Gonzalez, M, Reigel, B, Bobrow, B, Abella, B. Continuous chest compression cardiopulmonary resuscitation training promotes rescuer self-confidence and increased secondary training: A hospital-based randomized controlled trial, Crit Care Med 2012; 40(3):787-792. DOI: 10.1097/CCM.0b013e318236f2ca
- Burnett AM, Segal N, Salzman JG, McKnite MS, Frascone RJ, Potential Negative Effects of Epinephrine on Carotid Blood Flowand ETC02 during Active Compression-Decompression CPR utilizing an Impedance Threshold Device, Resuscitation (2010), doi:10.1016/j.resuscitation.2012.03.018
- Pozner, C, Almozlino, A, Elmer, J, Poole, S, McNamara, D, Barash, D. Cardiopulmonary resuscitation feedback improves the quality of chest compression provided by hospital health care professionals, The American Journal of Emergency Medicine 2011; 29:618-625. doi:10.1016/j.ajem.2010.01.008
- Kern, K, Stickney, R, Gallison, L, Smith, R. Metronome improves compression and ventilation rates during CPR on a manikin in a randomized trial, Resuscitation 2010; 81:206-210. doi:10.1016/j.resuscitation.2009.10.015
- Aufderheide, T, Frascone, R, Wayne, M, Mahoney, B, Swor, R, Domeier, R, Olinger, M, Holcomb, R, Tupper, D, Yannupoulos, D, Lurie, K. Standard cardiopulmonary resuscitation versus active compression-decompression cardiopulmonary resuscitation with augmentation of negative intrathoracic pressure for out-of-hospital cardiac arrest: a randomised trial, Lancet 2011; 377:301-311. DOI:10.1016/S0140- 6736(10)62103-4
- Maisch, S, Gamon, E, Ilisch, A, Goetz, A, Schmidt, G. Comparison of the over-the-head, lateral and alternating positions during cardiopulmonary resuscitation performed by a single rescuer with a bagevalveemask device, Emerg Med J 2011; 28:974-978. doi:10.1136/emj.2010.098251
- Yeung, J, Meeks, R, Edelson, D, Gao, F, Soar, J, Perkins, G. The use of CPR feedback/prompt devices during training and CPR performance: A systematic review, Resuscitation 2009; 80:743-751. doi:10.1016/j.resuscitation.2009.04.012
- Ettl, F, Testori, C, Weisner, C, Fleischhackl, S, Mayer-Stickler, M, Herkner, H, Schreiber, W, Fleischhackl, R. Updated teaching techniques improve CPR performance measures: A cluster randomized, controlled trial. Resuscitation 2011; 82:730-735. doi:10.1016/j.resuscitation.2011.02.005
- Yougquist, S, Niemann, J, Allread, G, Heyming, T, Rosborough, J. Neurologically Intact Survival in a Porcine Model of Cardiac Arrest: Manual Cardiopulmnary Resuscitation vs. LifeBelt Cardiopulmonary Resuscitation. Prehospital Emergency Care 2010; 14:324-328. doi: 10.3109/10903121003770662
- Emberger, J, Racine, L, Maheshwari, V. Lung Hernia Associated With Hemothorax Following Cardiopulmonary Resuscitation, Respir Care 2011; 56(7):1037-1039. DOI: 10.4187/respcare.01069
- Smekal, D, Johansson, J, Huzevka, T, Rubertsoon, S. A pilot study of mechanical chest compressions with the LUCASTM device in cardiopulmonary resuscitation, Resuscitation 2011; 82:702-706. doi:10.1016/j.resuscitation.2011.01.032
- Chung, T, Kim, S, You, J, Cho, Y, Chung, S, Park, I. A higher chest compression rate may be necessary for metronome-guided cardiopulmonary resuscitation, The American Journal of Emergency Medicine 2012; 30:226-230. doi:10.1016/j.ajem.2010.11.026
| Special Photo thanks to David Hunt and Joe Chacon of Superior Ambulance | |
| Post-faux-resuscitation David Hunt and John Korbin | |
